Hepatitis Function Panel (Part 2)
Dr. Joseph E. Graas, Scientific Director
Dr. Edward Moore, Medical Director
As stated in the previous edition of the Toxicology Times, drug, alcohol, and pesticides will cause both reversible and irreversible changes in the cellular structure of the liver. If the poisoning of the liver cells is severe, the clinical result will be acute chemical hepatitis and may evolve into necrosis and liver failure. If the offending chemical toxin occurs over a duration of time, the result may be scarring of the tissue with the laying down of fibrous tissue causing involution and shrinkage, often referred to as cirrhosis. In either case this damage restricts the flow of blood into and out of the liver, impeding the liver’s ability to eliminate and detoxify the body. Acutely you will see elevations of all of the liver enzymes, often 5-10 times the normal values, as well as increases in bilirubin that can be visually observed as the yellowing of the skin and whites of the eyes seen in jaundice. In chronic cases there may or may not be elevation of the liver enzymes, but more often, elevation of the bilirubin is seen. Clinically in the chronically cirrhotic liver one may see portal hypertension that results when blood cannot get through the liver and which will cause hemorrhoids, esophageal varices (hemorrhoids of the lower esophagus), splenomegaly with platelet sequestration (causing lower platelet count), and caput medusa (appearance of distended and engorged superficial veins) over the lower abdomen. As you can see, it is a challenge to assess the values in the Hepatic Function panel as they pertain to the status of liver health or liver disease.
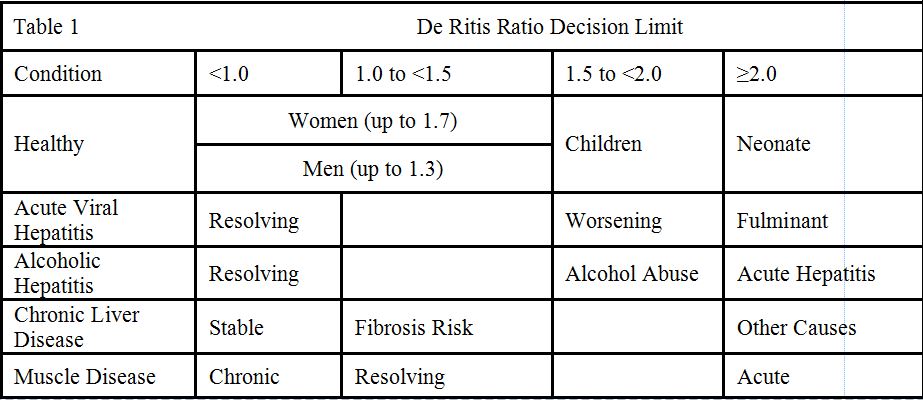
Medicine has been frustrated by the lack of a specific sensitive blood marker for alcohol consumption other than alcohol itself. Any damage to liver cells, whether caused by virus, bacteria, trauma, congestion with blood, or toxins (such as in the case of alcohol), will cause the liver cells to become leaky. This leads to the spilling of those enzymes located within the hepatic cells (hepatocytes) into the blood and a rise above the normal range detected in the laboratory. The markers for trauma to the hepatocytes are the enzymes GGT (Gamma Glutamyl Transferase, ALT (Alanine Aminotransferase), AST (Aspartate Aminotransferase) and in a more nonspecific way LDH (Lactate Dehydrogenase) and ALP (Alkaline Phosphatase). These enzymes are in other cell types and the serum values determined in the laboratory is a sum total of all of these, not just the liver hepatocytes. One of the enzymes, however, is specific to the liver and its increase will always be associated with liver damage despite what initially causes the damage. Alcohol damage is often looked for by measuring GGT, however, measuring the ratio of AST to ALT is more suggestive of damage by alcohol when the ratio is 2.0 or larger. This observation was published more than 50 years ago and is named after its author as the De Ritis Ratio (Clin Chem Acta. 1957, 2: 70-74). While simple clinical decision limits have been established for the De Ritis Ratio (e.g. >2.0 for alcoholic hepatitis or >1.0 for fibrosis/cirrhosis), there aren’t any generally accepted reference intervals for the ratio and indeed it is difficult to define ‘healthy’ limits for the ratio if its main application is when transaminases are abnormal. A summary of generally accepted interpretations is listed in table 1. Clin Biochem Rev 2013, Nov, 34(2): 117-130
Chemical toxins (alcohol, pesticides, etc.) and their effects on liver disease are not as simple as other diagnostic assessments of the liver function panel. As in the last issue of the Toxicology Times, we would refer you to your medical staff for a further and more complete interpretation and understanding of these results.
